A herniated disc is a condition in which the gel-like center of a vertebral disc protrudes through a weakened or damaged outer wall, causing pain and discomfort. This condition can affect people of all ages; however, certain factors increase the likelihood of developing a herniated disc.
One of the most common risk factors is age. As we get older, the discs in our spine start to lose water content and become less flexible, making them prone to herniation. Additionally, people who engage in repetitive activities that put pressure on the spine, such as heavy lifting or twisting motions, have a higher risk. Jobs that involve manual labor or specific sports that require excessive strain on the back also contribute to herniated discs.
Obesity is another significant risk factor. Excess weight puts added stress on the spine, increasing the chances of disc herniation. Poor posture, sedentary lifestyle, and weak abdominal muscles also contribute to this condition. Moreover, individuals with a family history of herniated discs are at a higher risk, as genetics can play a role in the integrity of the spinal discs.
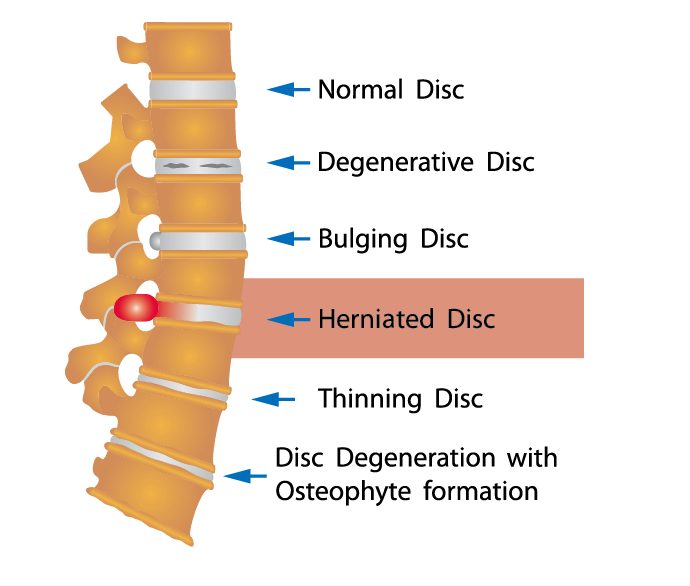
Certain health conditions can also predispose someone to herniated discs. Conditions like osteoporosis, which weakens the bones, and degenerative disc disease, which occurs with age-related disc wear and tear, can increase the likelihood of herniation. Lastly, smoking and lack of physical activity can also contribute to the development of herniated discs.
In conclusion, while a herniated disc can affect anyone, some factors increase the likelihood of developing this condition. Age, repetitive activities, obesity, poor posture, weak abdominal muscles, family history, certain health conditions, smoking, and lack of physical activity all contribute to the risk. Understanding these factors and taking preventative measures can help reduce the chances of a herniated disc occurrence.
What is the most common disc to herniate?
Most disk herniations happen in the lower lumbar spine, especially between the fourth and fifth lumbar vertebrae and between the fifth lumbar vertebra and the first sacral vertebra (the L4-5 and L5-S1 levels).
At what age do herniated discs start?
People ages 30 to 50 are most likely to get a herniated disk. The problem affects men twice as often as women.Jul 1, 2021
What is the number 1 most common cause of disc herniation?
The most common cause of disc herniation is a degenerative process in which, as humans age, the nucleus pulposus becomes less hydrated and weakens. This process will lead to a progressive disc herniation that can cause symptoms. The second most common cause of disc herniation is trauma.
What are 3 signs and symptoms of a herniated disk?
– Pain that occurs on one side of the body.
– Sharp pain in one part of the leg, hip, or buttocks and numbness in other parts. …
– Pain when moving your neck or deep pain near or over the shoulder blade.
What are the disadvantages of Microdiscectomy?
The main risks with microdiscectomy surgery are: infection. post-operative bleeding. blood clots (deep vein thrombosis or pulmonary embolism) pneumonia.
Is a Microdiscectomy a major or minor surgery?
Even though microdiscectomy recovery times are generally much faster than more invasive spinal surgeries, they’re still major procedures that involve general anesthetic. As such, they require careful oversight prior to medical personnel releasing you to return home. You can expect several specific things to happen.
Is lumbar discectomy considered as major surgery?
It’s increasingly common today for spine-related procedures to involve minimally invasive techniques. This is one of the reasons a discectomy isn’t necessarily “major” surgery in the traditional sense. Still, any spine-related procedure should be taken seriously, especially when it comes to recovery.Feb 4, 2022

How big is the incision for lumbar discectomy?
In a minimally invasive discectomy, a small incision (less than 1 inch) is made to one side of your back (Fig. 3). Next, a series of progressively larger dilators are passed, one around the other, to gradually separate the muscles and create a tunnel to the bony vertebra.

How long does a Microdiscectomy operation take?
The operation is usually performed under a general anaesthetic but various anaesthetic techniques are possible. The operation usually takes between 1 and 2 hours. Your surgeon will make a cut on the centre of your back between the vertebrae.