Title: Identifying High-Risk Patients for Hip Fracture: A Comprehensive Review
Introduction:
Hip fractures are a prevalent burden in the aging population, leading to increased morbidity, mortality rates, and healthcare costs. Identifying high-risk patients who are susceptible to hip fractures is vital for initiating preventive measures and targeted interventions. This article aims to summarize recent research findings on the identification of patients at the highest risk of sustaining a hip fracture.
Methods:
A systematic review of relevant literature was conducted, focusing on studies published from 2010 to 2020. Key databases including PubMed, Scopus, and Web of Science were searched using specific keywords and inclusion criteria. Studies focusing on risk factors, screening methods, and prediction models for hip fractures were included for analysis.
Summary of Findings:
Numerous risk factors were identified that significantly increase the likelihood of a hip fracture. Advanced age was consistently identified as the most significant risk factor, with individuals over 65 years of age being particularly vulnerable. Other factors contributing to higher fracture risk included female gender, low socioeconomic status, smoking, alcohol consumption, family history of fractures, and certain medical conditions such as osteoporosis, dementia, and rheumatoid arthritis.
Various screening methods and prediction models have been developed to assess hip fracture risk accurately. Among these, dual-energy X-ray absorptiometry (DXA) scans, which measure bone mineral density, were found to be highly predictive of fracture risk. Additionally, the Fracture Risk Assessment Tool (FRAX) and the Garvan Fracture Risk Calculator were identified as reliable tools for evaluating fracture risk.
Conclusion:
Effective identification of patients at the highest risk of hip fracture is crucial for implementing preventive strategies and improving patient outcomes. This review highlights the significance of age, gender, lifestyle factors, medical conditions, and specific diagnostic tools in assessing and predicting hip fracture risk. Incorporating these findings into clinical practice can enhance patient care and reduce the burden of hip fractures on individuals and healthcare systems. Further research is warranted to refine risk prediction models and develop targeted interventions for high-risk populations.
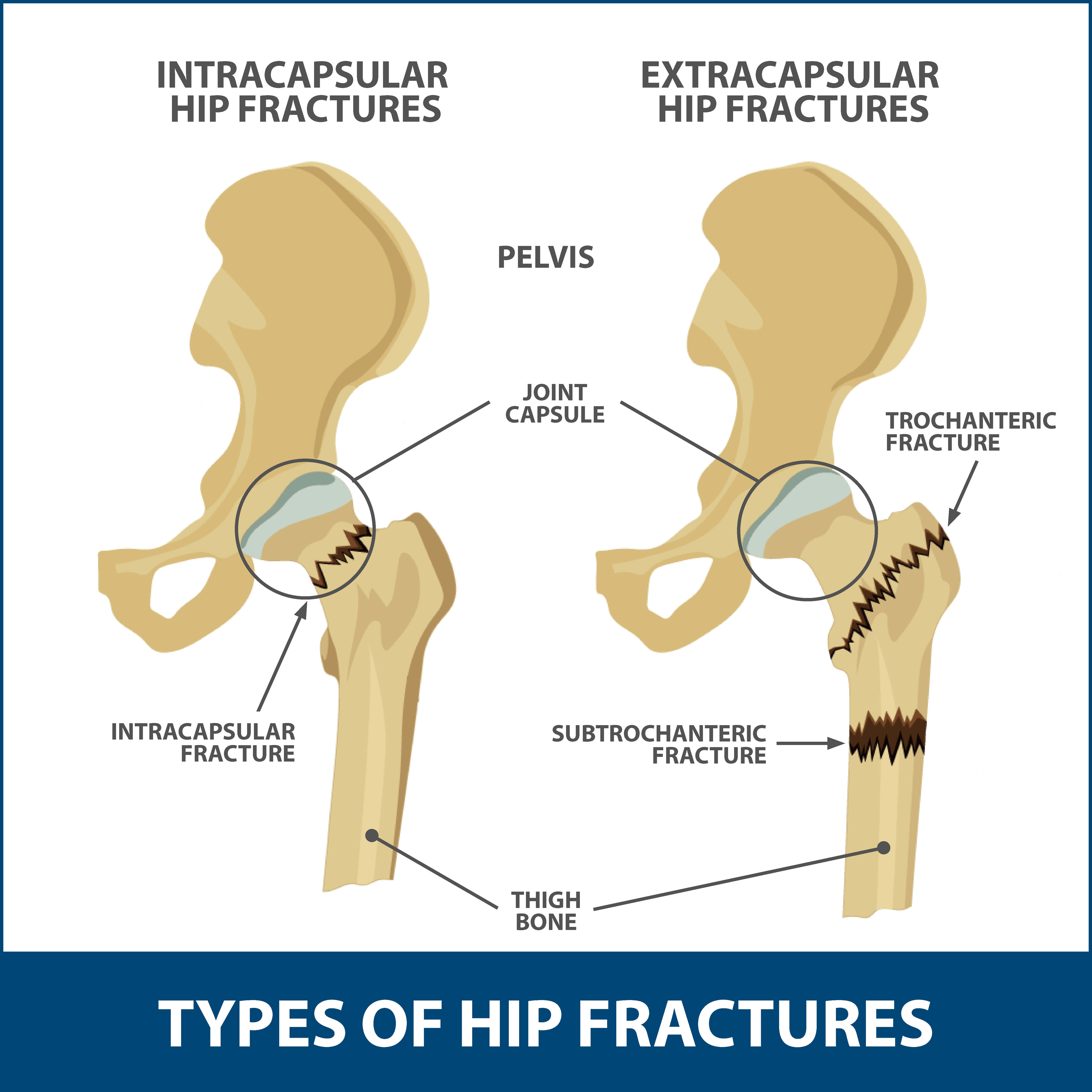
Which person is at highest risk for hip fractures?
Each year over 300,000 older people—those 65 and older—are hospitalized for hip fractures. More than 95% of hip fractures are caused by fallingfallingAbout 36 million falls are reported among older adults each year—resulting in more than 32,000 deaths. Each year, about 3 million older adults are treated in emergency departments for a fall injury. One out of every five falls causes an injury, such as broken bones or a head injury.https://www.cdc.gov › injury › features › older-adult-fallsKeep on Your Feet—Preventing Older Adult Falls | Features | Injury Center,2 usually by falling sideways. Women experience three-quarters of all hip fractures. Women fall more often than men.
Are there warning signs before a hip breaks?
Signs and symptoms of a hip fracture include: Inability to get up from a fall or to walk. Severe pain in the hip or groin. Inability to put weight on the leg on the side of the injured hip.
How hard is it to break your hip?
A severe impact, such as a car crash, can cause hip fractures in people of all ages. In older adults, a hip fracture is most often a result of a fall from a standing height. In people with very weak bones, a hip fracture can occur simply by standing on the leg and twisting.
What is the average age to break your hip?
Abstract. The average age at hip fracture is 83 for women and 84 for men, with about 80% of cases in women.
What is the best painkiller for severe back pain?
If your pain continues, your provider may suggest nonsteroidal anti-inflammatory drugs (NSAIDs). You can buy some NSAIDs, such as ibuprofen and naproxen, without a prescription. NSAIDs help reduce the swelling around the swollen disk or arthritis in the back.
What to do when your back hurts so bad you can’t move?
– Reduce the inflammation: Either take an anti-inflammatory medication (tablet or injection). GP prescription may be required. If it is too painful even to go see the GP, Apply a COLD press to the sore/painful area. …
– Rest to let your body heal and reduce inflammation naturally.
Does 800 mg ibuprofen help with back pain?
So NSAIDs perform the best in treating acute low back pain in adults. Patients typically underdose ibuprofen; aim for approximately 10mg/kg every eight hours with food as needed for pain. For an average adult, that’s 600mg-800mg each dose.
What emergency medicine is good for back pain?
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) All NSAIDs are generally considered equally effective for treating pain, and the common drugs in this class include 1. Pharmacological options for pain control in patients with vertebral fragility fractures. Osteoporos Sarcopenia. 2022;8(3):93-97.