Diabetic neuropathy is a common complication of diabetes mellitus that affects the nerves and can lead to various symptoms such as pain, tingling, and numbness in the extremities. Understanding what triggers this condition is essential for effective management and prevention strategies.
One of the leading factors that triggers diabetic neuropathy is prolonged exposure to high blood sugar levels. Chronically elevated glucose levels can contribute to nerve damage by impairing blood flow and reducing the delivery of essential nutrients to the nerves. This, in turn, leads to nerve dysfunction and the development of neuropathy symptoms.
Another significant trigger is inflammation. Inflammation in the body has been associated with nerve damage and can further aggravate diabetic neuropathy. Chronic inflammation is often observed in individuals with poorly controlled diabetes, as high blood sugar levels can promote the release of pro-inflammatory chemicals.
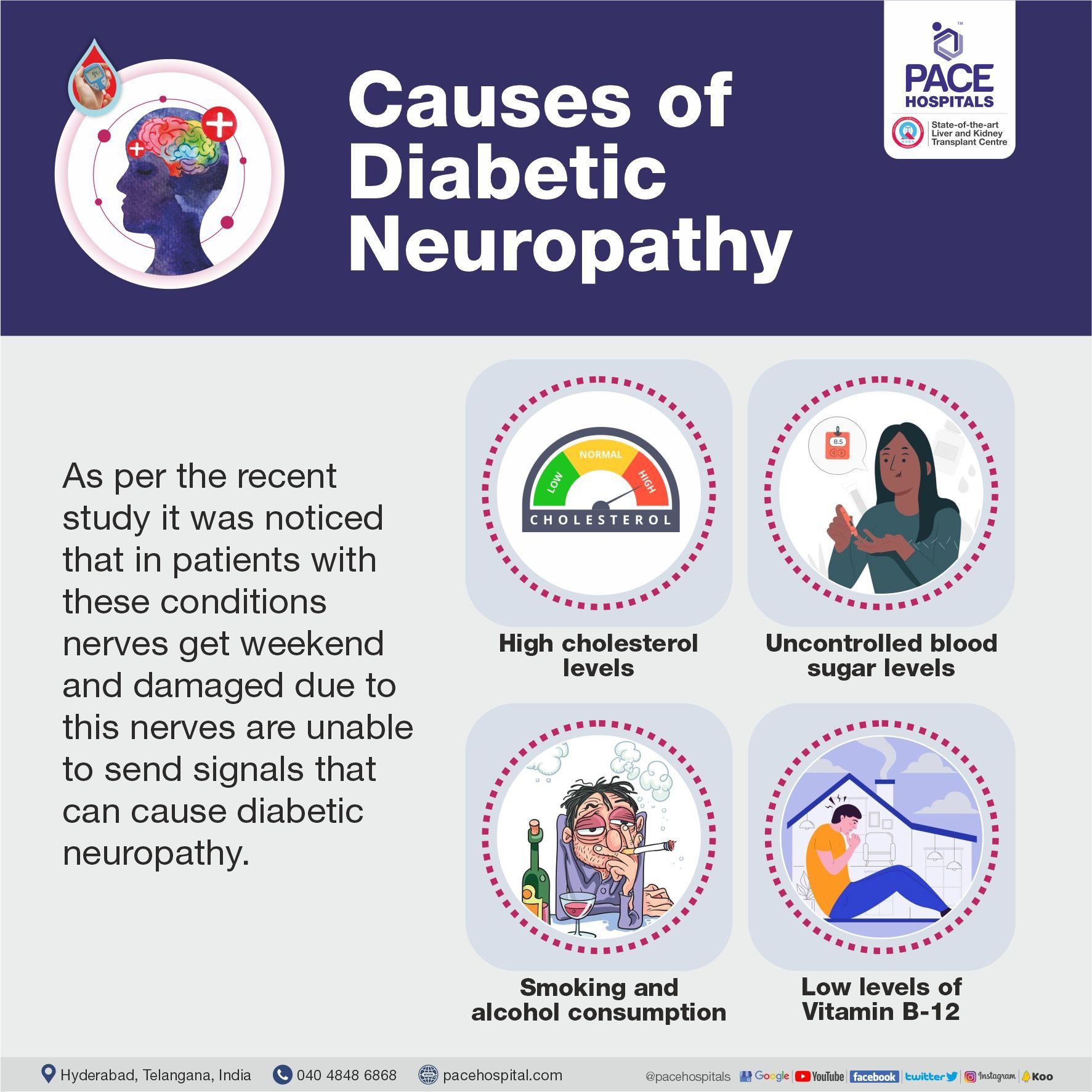
Additionally, certain lifestyle factors can contribute to the development of diabetic neuropathy. These include smoking, excessive alcohol consumption, and a sedentary lifestyle. Smoking, for example, has a detrimental effect on blood circulation, exacerbating nerve damage caused by elevated blood sugar levels.
Furthermore, other medical conditions such as high blood pressure, high cholesterol levels, and obesity can contribute to the development and progression of diabetic neuropathy. These conditions often coexist with diabetes and can further damage nerves, increasing the risk of neuropathy.
Genetic factors may also play a role in the susceptibility to diabetic neuropathy. Some individuals may have a genetic predisposition that increases their likelihood of developing this condition compared to others.
In conclusion, diabetic neuropathy is triggered by a combination of factors including prolonged exposure to high blood sugar levels, inflammation, lifestyle choices, coexisting medical conditions, and genetic predisposition. Understanding these triggers is crucial in implementing effective preventive measures and managing the condition in individuals with diabetes. Maintaining optimal blood sugar control, adopting a healthy lifestyle, and managing associated medical conditions are key components of managing diabetic neuropathy.
What causes diabetic neuropathy?
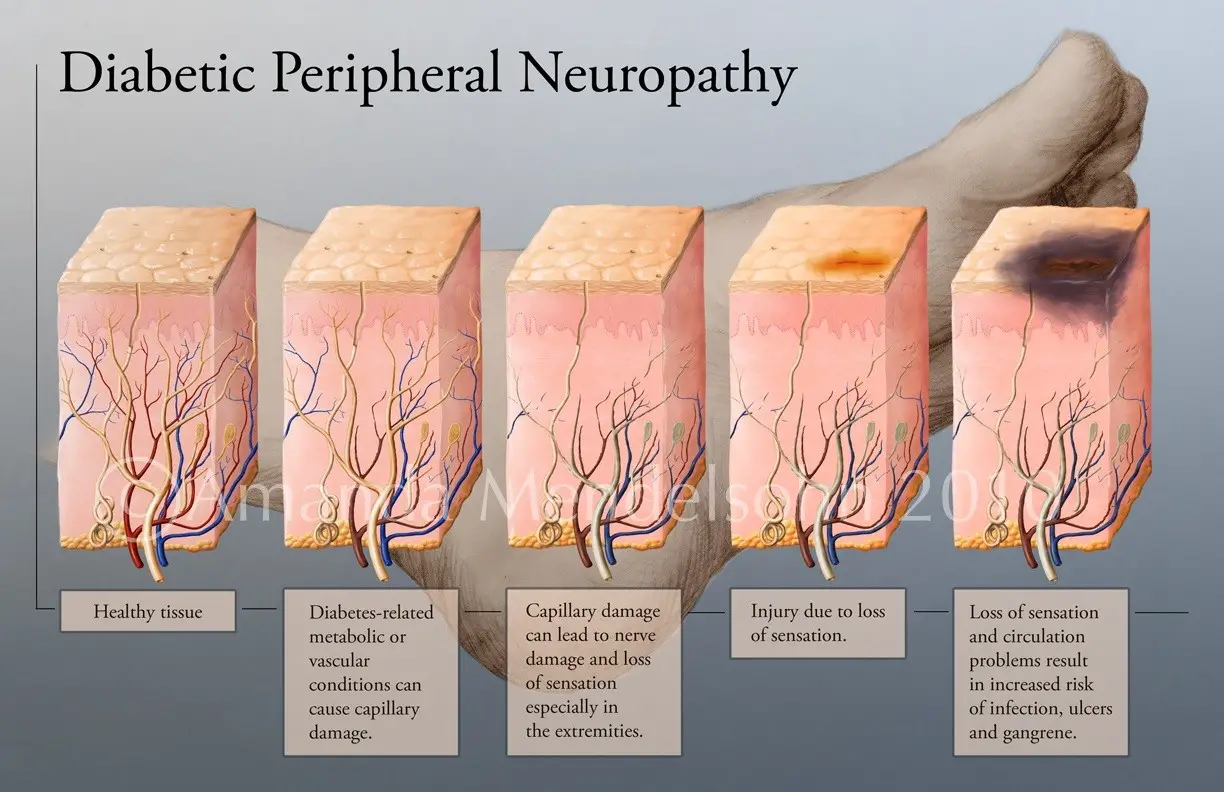
Neuropathy is one of the long-term complications of diabetes. Over time, high blood glucose (sugar) levels can damage the small blood vessels that supply the nerves in your body. This stops essential nutrients reaching the nerves. As a result, the nerve fibres can become damaged, and they may disappear.
What is the main cause of diabetic neuropathy?
Causes of diabetic neuropathy Over time, high blood glucose (sugar) levels can damage the small blood vessels that supply the nerves in your body. This stops essential nutrients reaching the nerves. As a result, the nerve fibres can become damaged, and they may disappear.
What are the three most common symptoms of diabetic neuropathy?
Signs and symptoms of peripheral neuropathy are often worse at night, and may include: Numbness or reduced ability to feel pain or temperature changes. Tingling or burning feeling. Sharp pains or cramps.
What are the stages of diabetic neuropathy?
– Stage One: Numbness & Pain. In this beginning stage, patients become aware that something feels “off” with the nerves in their hands and/or feet. …
– Stage Two: Constant Pain. …
– Stage Three: Intense Pain. …
– Stage Four: Complete Numbness/ Loss of Sensation.
How do you release a pinched nerve in your shoulder?
You can take some easy measures to sort out this pain at home. One helpful treatment for shoulder nerve pain is getting into a warm, cosy bed and having some rest. You could also try a hot or cold compress on your shoulder as you watch TV or relax. A soft cervical collar may also help by immobilising your neck.
How do I know if my shoulder pain is nerve related?
Signs & Symptoms of a Pinched Nerve in the Shoulder A pinched nerve typically causes pain, numbness, or discomfort in the shoulder area. Other symptoms that may accompany these changes include: Muscle weakness in the shoulder; this weakness may also extend into the hand and arm.
How do you get instant relief from a pinched nerve?
Apply ice and heat. Along with rest, ice and heat can ease pain from a pinched nerve. You don’t need anything fancy.
What does nerve pain in shoulder feel like?
A pinched nerve in the shoulder may cause pain, tingling, numbness, or discomfort, radiating from the shoulder into the arm, chest, or trapezius (trap) muscles. A person may also have other symptoms, which include: changes in feeling on the same side as the shoulder that hurts.
How do you massage a pinched nerve in your shoulder?
Self-massage techniques such as effleurage strokes to warm the muscles in the affected area followed by light kneading over any knots can help release tension in muscles. Once the muscles are relaxed, this may relieve pressure on the nerve and reduce the symptoms of pinched nerve.Jan 3, 2019