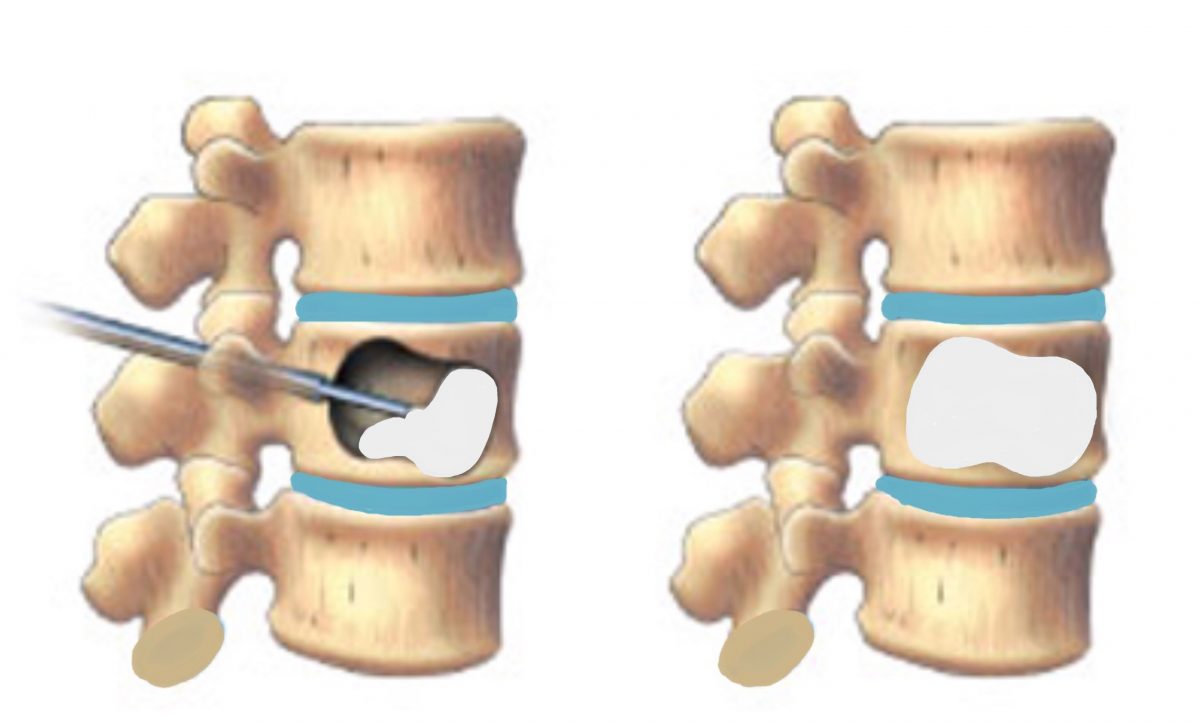
Kyphoplasty is a minimally invasive procedure used to treat vertebral compression fractures, which are often caused by osteoporosis. The success rate of kyphoplasty is generally high, with studies reporting rates of pain relief ranging from 70% to 90%. The procedure involves the insertion of a balloon into the fractured vertebra, which is then inflated to create a cavity. The cavity is filled with bone cement to stabilize the vertebra and reduce pain.
Several factors can affect the success rate of kyphoplasty, including the severity of the fracture, the skill of the surgeon, and the overall health of the patient. In some cases, additional procedures may be necessary to achieve the desired outcome. Despite these factors, kyphoplasty is generally considered to be a safe and effective treatment for vertebral compression fractures.
Overall, kyphoplasty has been shown to significantly improve pain levels and quality of life for patients with vertebral compression fractures. It is important for patients to discuss the potential risks and benefits of kyphoplasty with their healthcare provider to determine if it is the right treatment option for them.
What is the survival rate for kyphoplasty?
The study reported high survival rates in the kyphoplasty group at 1 and 3 years (85.2% and 59.9%, respectively), and even in patients stratified by age, compared with nonoperative (73.1% and 42.3%, respectively) and vertebroplasty (78.8% and 49.7%, respectively) groups.
How successful is kyphoplasty?
What is the success rate of kyphoplasty? An estimated 92% of people who undergo kyphoplasty report better pain relief after the procedure.
Why does my back still hurt after kyphoplasty?
The findings revealed that 7.8% of the 809 people included in the study still had back pain after the kyphoplasty. Independent risk factors for the continued pain included: having a cavity inside a fractured vertebra. swelling due to fluid being trapped behind the membrane covering the back muscles.
What are the drawbacks of kyphoplasty?
Some general surgical risks apply to kyphoplasty, including infection, excessive bleeding, and/or a negative reaction to anesthesia.
What is the primary treatment for a mallet finger?
Wearing a splint on your finger to keep it straight is the most common treatment for mallet finger. You may need to wear a splint for different lengths of time. If your tendon is only stretched, not torn, it should heal in 4 to 6 weeks if you wear a splint all the time.
How do you immobilize a mallet finger?
Usually, the finger is splinted in full extension (typically, 0 to 10 degrees extension) at the DIP joint for 6 to 8 weeks. This is followed by part-time splinting for an additional 4 to 6 weeks. Numerous types of splints have been used for mallet finger injuries.

Can you fix mallet finger at home?
Probably not. Most of the time, a mallet finger can be fixed by using an orthosis (or splint) that holds it straight for a several weeks; however, sometimes it can be more serious, which is why it is a good idea to have it professionally evaluated.
How do you repair a mallet finger?
Wearing a splint on your finger to keep it straight is the most common treatment for mallet finger. You may need to wear a splint for different lengths of time. If your tendon is only stretched, not torn, it should heal in 4 to 6 weeks if you wear a splint all the time.
What is the splinting protocol for mallet finger?
All mallet finger splints are designed to maintain full extension or slight hyperextension at the DIP joint. Commonly used splints are plastic stack splints, thermoplastic, and aluminum form splints. The authors recommend full time splinting for 6 weeks, followed by 2–6 weeks of splinting at night (Fig. 3).


