Sciatica is a condition that occurs when the sciatic nerve becomes compressed or irritated, leading to pain, numbness, and tingling in the lower back, buttocks, and legs. While conservative treatments such as physical therapy, medication, and injections are often effective in managing sciatica, surgery may be necessary for some individuals who do not find relief with these methods.
The best surgery for sciatica depends on the underlying cause of the condition. The most common surgical procedures for sciatica include discectomy, laminectomy, and spinal fusion. Discectomy involves removing all or part of a herniated disc that is pressing on the sciatic nerve. Laminectomy is a procedure in which a portion of the vertebrae is removed to relieve pressure on the nerve. Spinal fusion involves fusing two or more vertebrae together to stabilize the spine and reduce pressure on the nerve.
The success of surgery for sciatica depends on various factors, including the individual’s overall health, the severity of the condition, and the skill of the surgeon. It is important for individuals considering surgery for sciatica to discuss the risks and benefits with their healthcare provider and to explore all possible treatment options before making a decision. Surgery should be considered as a last resort when conservative treatments have not provided relief and when the pain and symptoms significantly impact the individual’s quality of life.
Is surgery the last resort for sciatica?
Many people get significant relief from sciatic symptoms with nonsurgical treatment options. However, if your pain and symptoms persist despite these treatments, Dr. Kellogg offers spine surgery for relief. Surgery is often the last resort because it’s invasive and requires anesthesia.
What is the new procedure for sciatica?
In pulsed RF, doctors use CT scans to slide a fine needle precisely into the nerves that are causing sciatic pain. The needle is then heated using pulses of radio waves. The heat disrupts the nerve, preventing it from sending pain signals to the brain. “It is similar to a reset of an operating system,” Napoli said.
What is the false negative rate for TB test?
TUBERCULIN SKIN TESTING TST has substantial limitations that diminish its value in diagnosing pulmonary TB. The TST lacks sensitivity and specificity. Prior to the emergence of HIV, false-negative TSTs among patients with pulmonary TB were well recognized and reported to occur in over 2% of patients.
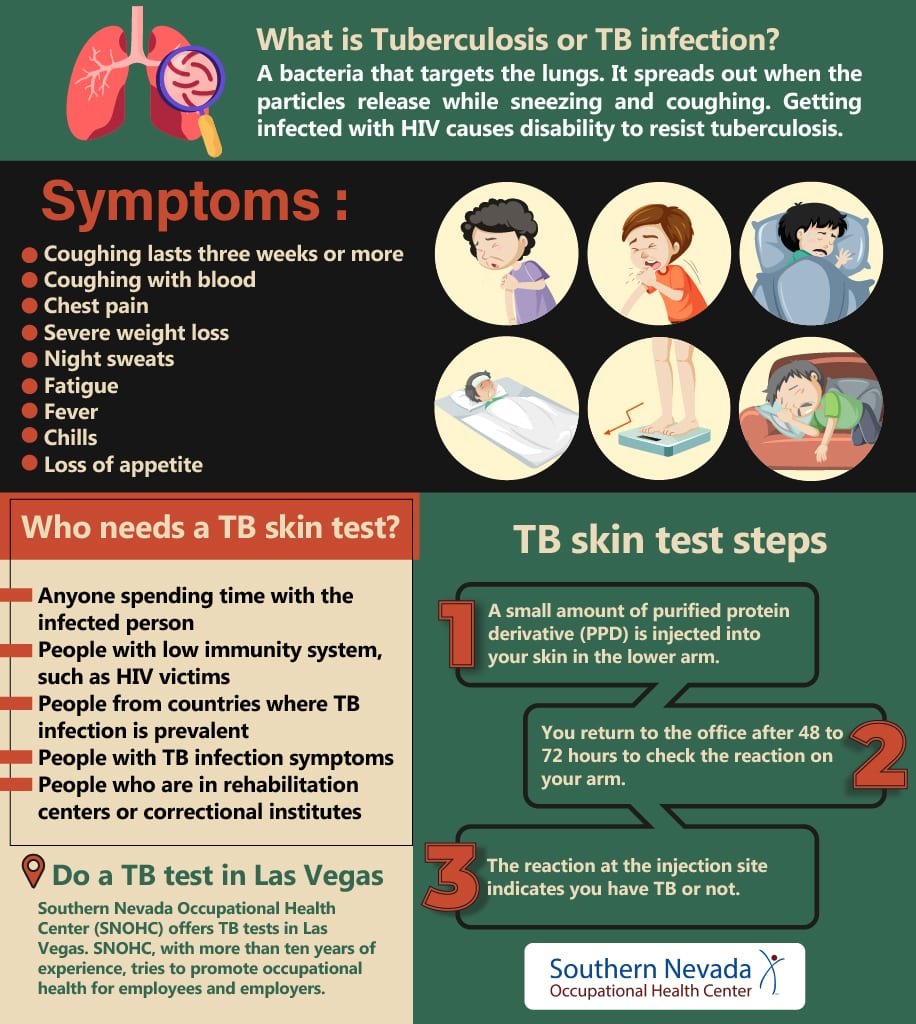
How accurate is the TB skin test?
TB skin: Subjective results. Requires 2 separate appointments and manual results. Sensitivity of 79% and specificity of 97% with specificity being as low as 59% in BCG-vaccinated patients (high false positive).
Can a blood test for TB be wrong?
Antibodies may also develop against other organisms which again could wrongly indicate they have active TB. In addition, different organisms share the same antigens, making tests results unreliable. These factors can result in TB disease not being identified or wrongly diagnosed.
How accurate is the tuberculin skin test?
TB skin: Subjective results. Requires 2 separate appointments and manual results. Sensitivity of 79% and specificity of 97% with specificity being as low as 59% in BCG-vaccinated patients (high false positive).
Is TB skin test more accurate than blood test?
Want a better test for TB infection? Then you want a TB blood test! The TB blood test is more specific than a TB skin test (less likely to cause a false positive) and it requires only one visit, while a TB skin test may require several visits (four visits over a 10 to 21 day period for a two-step test).

