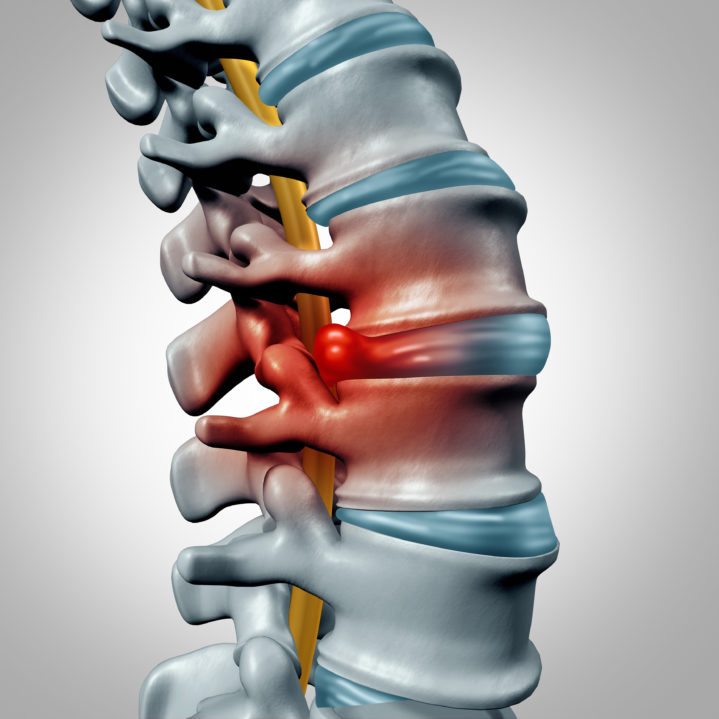
L5-S1 disc collapse refers to the degeneration or wear and tear of the intervertebral disc located between the fifth lumbar vertebra (L5) and the first sacral vertebra (S1) in the lower back. This condition can cause various symptoms that may vary in severity from person to person.
One of the most common symptoms of L5-S1 disc collapse is lower back pain. This pain can range from mild to severe and may be felt as a dull ache or a sharp, shooting sensation. Patients may experience difficulty in standing up straight or bending forward, and the pain may worsen with certain movements such as lifting heavy objects or twisting the spine.
In addition to lower back pain, L5-S1 disc collapse can also cause sciatica. Sciatica refers to pain that radiates down the buttocks and legs, often following the path of the sciatic nerve. This pain can be accompanied by numbness, tingling, or weakness in the affected leg. Patients may find it more comfortable to sit or lie down, as prolonged standing or walking can exacerbate the symptoms.
Other symptoms that may indicate L5-S1 disc collapse include decreased range of motion in the lower back, muscle weakness in the legs, and difficulty walking or maintaining balance. Some patients may also experience bladder or bowel dysfunction, although this is less common.
It is important to promptly seek medical attention if these symptoms arise, as untreated L5-S1 disc collapse can lead to further complications such as nerve damage and permanent disability. A healthcare professional will conduct a thorough physical examination, including diagnostic tests such as X-rays or MRI scans, to confirm the diagnosis and determine the appropriate treatment.
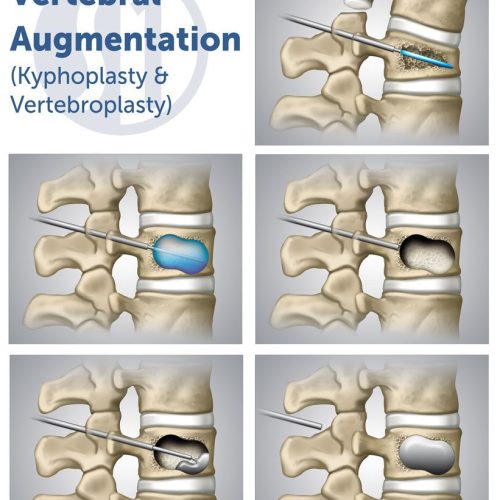
Treatment options for L5-S1 disc collapse may include pain management with medications or physical therapy to strengthen the supporting muscles and improve flexibility. In more severe cases, surgical intervention may be necessary to repair or replace the damaged disc.
Overall, the symptoms of L5-S1 disc collapse can significantly impact an individual’s daily life and mobility. Seeking timely medical intervention and following a comprehensive treatment plan can help alleviate symptoms and improve the overall quality of life for affected individuals.
What can be done for L5-S1 degenerative disc?
– Prescription and over-the-counter (OTC) medication may help reduce lower back and leg pain.
– Chiropractic adjustments may help relieve lumbar pain.
– Using a supported posture while bending and lifting helps protect the spinal structures.
– Epidural steroids help control inflammation around the spinal nerve roots.
Is walking good for L5-S1 disc?
Low-impact movements, such as walking, swimming, using a stationary bike, and cycling, are ideal because they minimize the stress on the injured disc.
How do you fix a herniated disc with L5-S1?
Can an L5-S1 disc bulge heal on its own? In some cases, mild disc bulges can improve with conservative treatments such as rest, physical therapy, and pain management. However, severe or persistent cases may require more aggressive interventions like injections or surgery.Aug 2, 2023
What activities should you avoid with L5-S1?
Avoid activities that require frequent twisting and bending, such as golfing or gardening, or even handling heavy objects at work without employing proper lifting techniques. Sitting down for prolonged periods of time: Prolonged sitting can put pressure on the L5-S1 disc and increase pain and stiffness levels.Apr 5, 2023
What worsens a herniated disc?
Coughing, sneezing, sitting, driving, and bending forward may make the pain worse. The pain gets worse when you make these movements because there is more pressure on the nerve. People with painful herniated discs often try to change positions to reduce the pain.
What is the fastest way to heal a herniated disc?
Self care: In most cases, the pain from a herniated disc will get better within a couple days and completely resolve in 4 to 6 weeks. Restricting your activity, ice/heat therapy, and taking over the counter medications will help your recovery.
What not to do with a herniated disc?
– Sitting too much. Sitting puts more stress on your spinal discs, especially when slouching forward in a seat. …
– Doing laundry. …
– Vacuuming. …
– Feeding a pet. …
– Strenuous exercise. …
– Shoveling snow or gardening.
Is stretching good for herniated disc?
A herniated or bulging disc can lead to muscle spasms in your back. Thus, it’s recommended that you stretch your muscles as often as possible to ease the pain and prevent muscle spasms from becoming chronic. There are many great stretches that you can do to ease the back pain caused by a herniated disc.
What activity restrictions for herniated disc?
– Sitting too much. Sitting puts more stress on your spinal discs, especially when slouching forward in a seat. …
– Doing laundry. …
– Vacuuming. …
– Feeding a pet. …
– Strenuous exercise. …
– Shoveling snow or gardening.