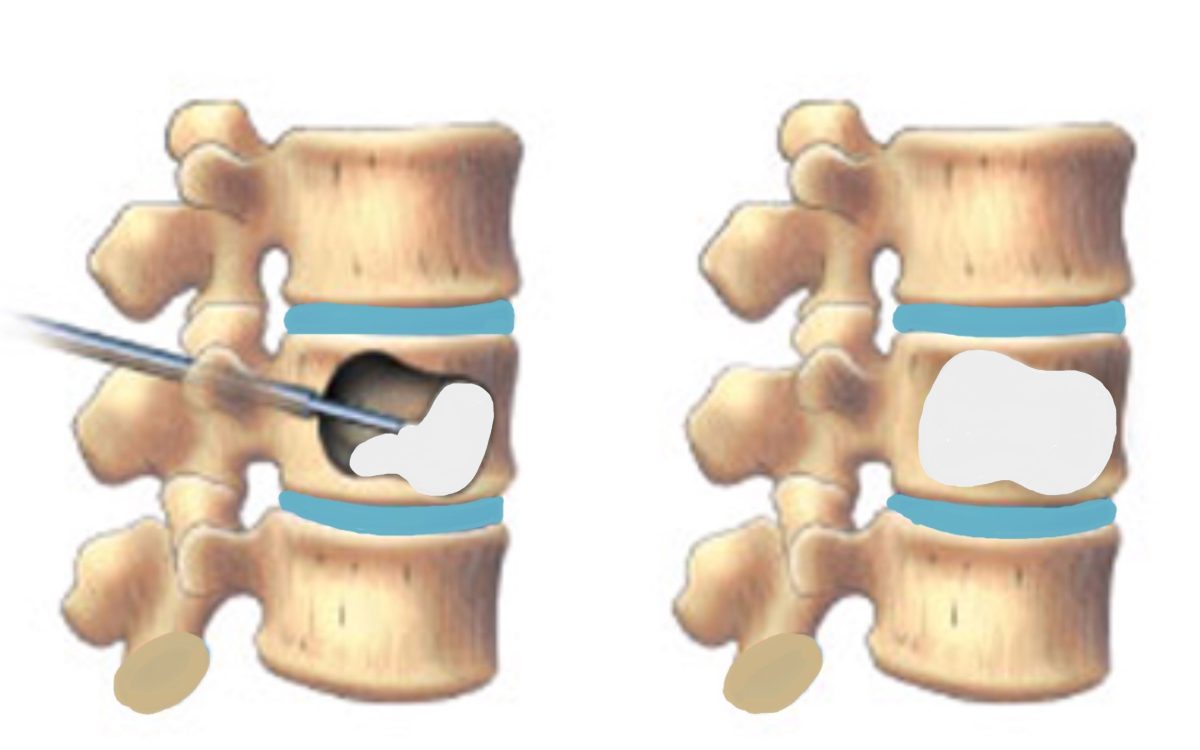
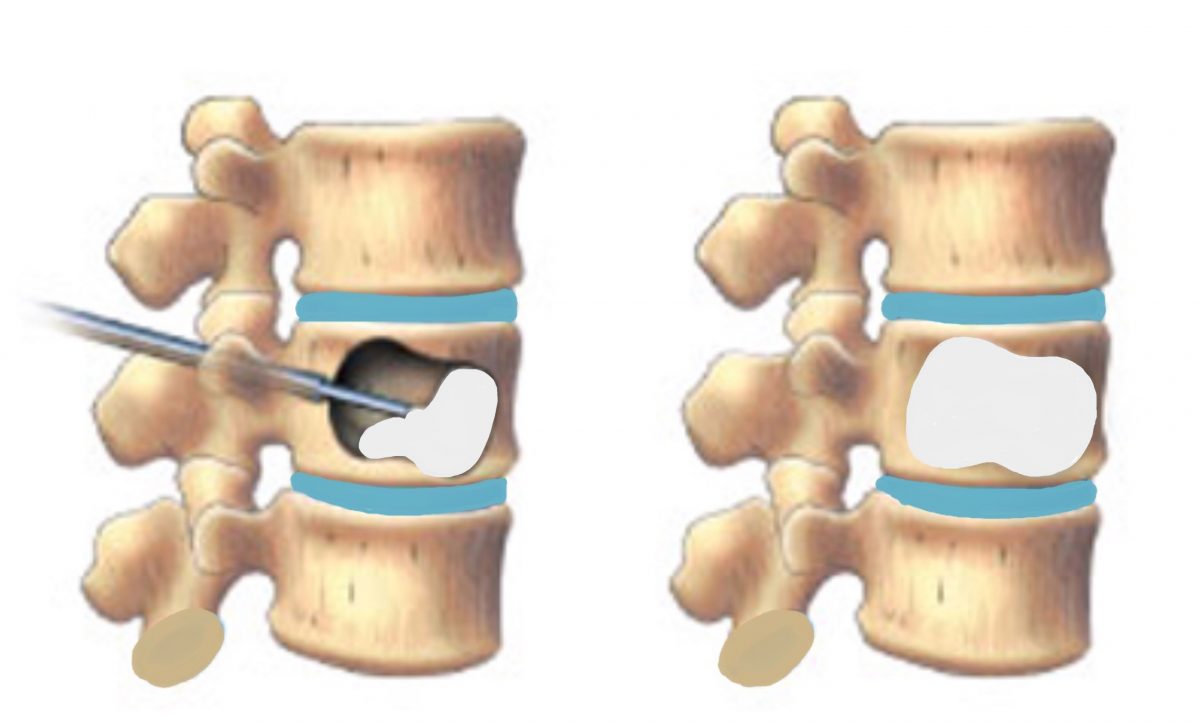
Kyphoplasty is a minimally invasive procedure used to treat vertebral compression fractures in the spine. Although it involves the use of local anesthesia and sedation, it is generally considered to be a minor surgery compared to traditional open surgeries. During kyphoplasty, a small incision is made in the back and a balloon is inserted into the fractured vertebra. The balloon is then inflated to create space and restore the vertebra to its normal height. Once the space is created, bone cement is injected into the vertebra to stabilize it and alleviate pain.
Kyphoplasty is typically performed on an outpatient basis, meaning patients can usually go home the same day as the procedure. Recovery time is relatively quick, with patients often experiencing significant pain relief within a few days. While kyphoplasty is generally safe and effective, like any surgical procedure, there are some risks involved, such as infection, nerve damage, or allergic reaction to anesthesia. It is important for patients to discuss these risks with their doctor before undergoing kyphoplasty. Overall, kyphoplasty is a valuable treatment option for individuals suffering from vertebral compression fractures, offering a less invasive alternative to traditional surgery.
What is the success rate of kyphoplasty?
What is the success rate of kyphoplasty? An estimated 92% of people who undergo kyphoplasty report better pain relief after the procedure.
What is the survival rate for kyphoplasty?
The study reported high survival rates in the kyphoplasty group at 1 and 3 years (85.2% and 59.9%, respectively), and even in patients stratified by age, compared with nonoperative (73.1% and 42.3%, respectively) and vertebroplasty (78.8% and 49.7%, respectively) groups.
Why does my back still hurt after kyphoplasty?
The findings revealed that 7.8% of the 809 people included in the study still had back pain after the kyphoplasty. Independent risk factors for the continued pain included: having a cavity inside a fractured vertebra. swelling due to fluid being trapped behind the membrane covering the back muscles.
What are the drawbacks of kyphoplasty?
Some general surgical risks apply to kyphoplasty, including infection, excessive bleeding, and/or a negative reaction to anesthesia.
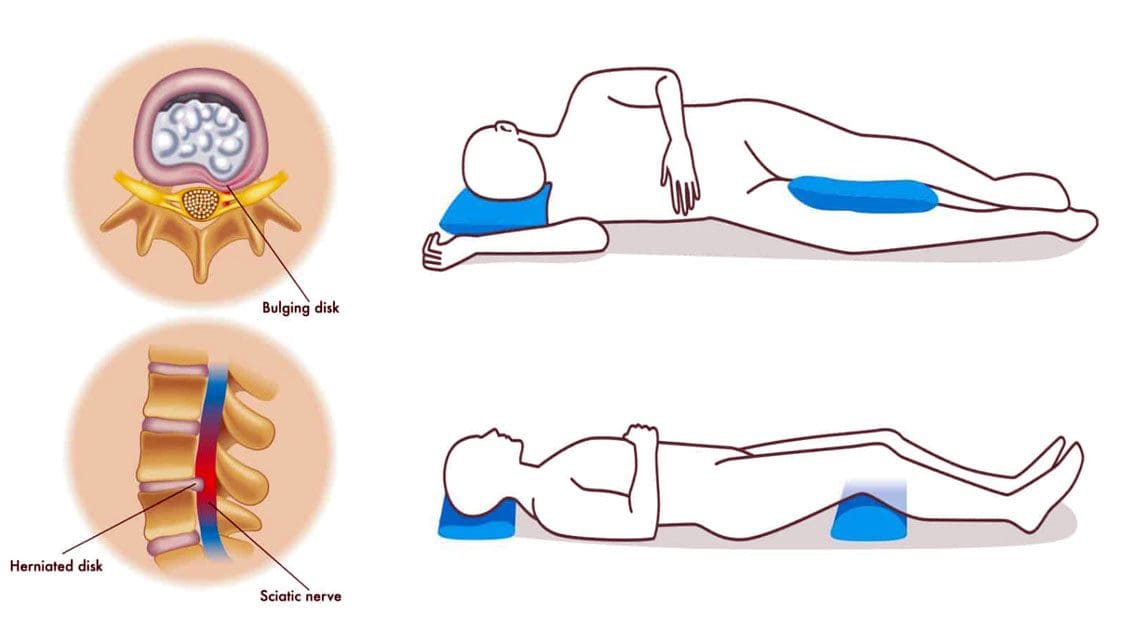
How long is the rest for a slipped disc?
Most people recover from a slipped disc within six weeks without treatment. Until then there are a number of treatment options that aim to help relieve the pain and improve mobility.Apr 9, 2020
Is bed rest required for slip disc?
How long should bedrest be used when treating a slipped disc? For patients with neck pain radiating down the arm and a diagnosis of herniated disc, there is no need or indication for strict bed rest. Certainly, a day of two of taking it easy and staying in bed is fine but it should not be done for more than that.
Does slipped disc pain ever go away?
5. Slipped discs usually resolve on their own, but physical therapy or other medications can help with pain. The majority of disc herniations improve on their own within six weeks to three months, as the body releases enzymes to clear away the herniated piece and the pressure on the nerves goes away.Mar 8, 2022
Is a slipped disc for life?
Herniated disks get better on their own over time or with nonsurgical treatment for 9 out of 10 people. If other treatments don’t relieve your symptoms, your healthcare provider may recommend surgery.Jul 1, 2021

Can you fully recover from a slipped disk?
Unfortunately, there is no clear-cut answer as to whether your disc herniation will fully heal. With treatment, a disc herniation can dry up, shrink or go away. Your body may have an autoimmune response and aid in healing the herniation.Oct 6, 2022