A clavicle fracture is an acute injury that occurs when the collarbone, located between the shoulder blade and breastbone, breaks. This type of injury is typically caused by a direct blow to the shoulder or a fall onto an outstretched arm. The most common symptom of a clavicle fracture is severe pain, swelling, and bruising at the site of the break. In some cases, the skin may even appear to be tenting over the broken bone.
Treatment for a clavicle fracture usually involves immobilizing the arm and shoulder with a sling or brace to allow the bone to heal properly. In some cases, surgery may be required to realign the broken bone and stabilize it with pins or plates. Physical therapy is often recommended after the initial healing period to help restore strength and range of motion to the shoulder.
It is important to seek prompt medical attention if you suspect you have a clavicle fracture, as delaying treatment can lead to complications such as improper bone healing or nerve damage. With proper care and rehabilitation, most people with a clavicle fracture can expect to make a full recovery and return to their normal activities within a few months.
What is the approach to a midshaft clavicle fracture?
Nonoperative treatment is preferred for nearly all acute, nondisplaced midshaft clavicle fractures. Treatment with an arm sling is preferred over a figure-of-eight dressing for acute midshaft clavicle fractures because it is better tolerated and leads to similar outcomes.Jan 1, 2008
What is a Grade 3 fracture of the clavicle?
Type 3 fracture is where there is non-displacement of the fracture but it extends into the acromioclavicular joint. Again, these fractures are treated non-surgically. However, late AC degenerative changes can occur and may require excision of the distal clavicular segment.
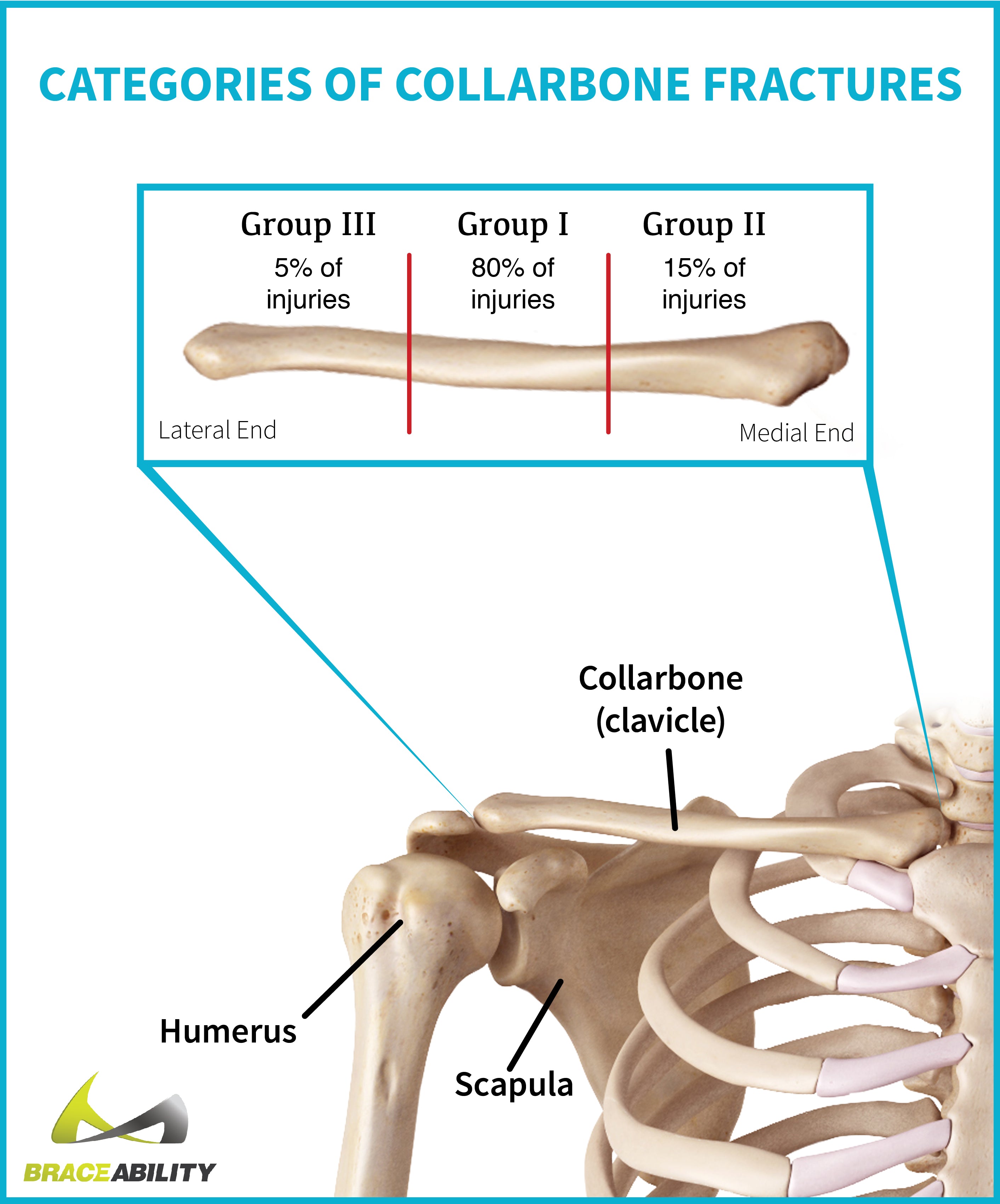
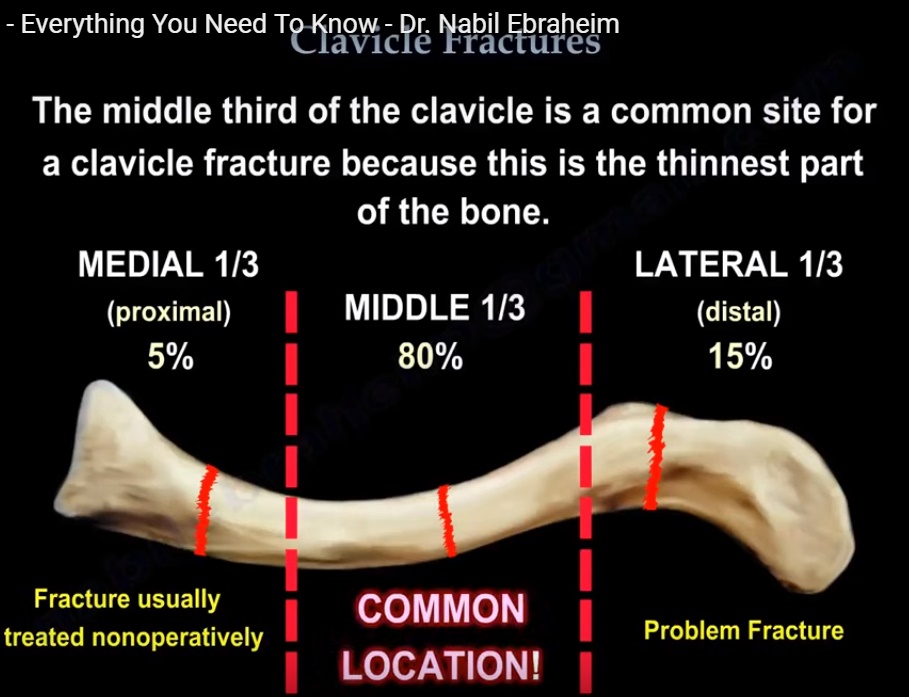
What is the classification of clavicular fractures?
The anatomic site of the fracture is typically described using the Allman classification, which divides the clavicle into thirds. Group I (midshaft) fractures occur on the middle third of the clavicle, group II fractures on the lateral (distal) third, and group III fractures on the medial (proximal) third.Jan 1, 2008
How is a proximal clavicle fracture treated?
Most clavicle fractures are treated conservatively and nonoperatively. Patients are immobilized in a sling or figure-of-eight brace until the clinical union is achieved. This typically occurs by 6 to 12 weeks in adults and 3 to 6 weeks in children.
Is a kyphoplasty a major surgery?
Kyphoplasty is considered a minimally invasive surgery because it is performed through a small skin puncture rather than a larger (open) incision. A typical kyphoplasty procedure, described below, takes 1 to 2 hours per vertebral level to complete.
What do you do for a l1 compression fracture?
Most compression fractures due to injury heal in 8 to 10 weeks with rest, wearing of a brace, and pain medicines. However, recovery can take much longer if surgery was done. You will lose some height and have a more bent back. Fractures due to osteoporosis often become less painful with rest and pain medicines.
How painful is kyphoplasty?
Most kyphoplasty procedures take less than an hour. Once it’s complete, we monitor you for a while to make sure you’re feeling okay. Although you might feel a little soreness at the incision site, the procedure causes very little tissue damage, and minor discomfort goes away quickly.
Are you put to sleep for kyphoplasty?
You may have local anesthesia (awake and unable to feel pain). You will likely also receive medicine to help you relax and feel sleepy. You may receive general anesthesia. You will be asleep and unable to feel pain.
What is l1 kyphoplasty?
kyphoplasty: a minimally invasive procedure used to treat vertebral compression fractures by inflating a balloon to restore bone height then injecting bone cement into the vertebral body.