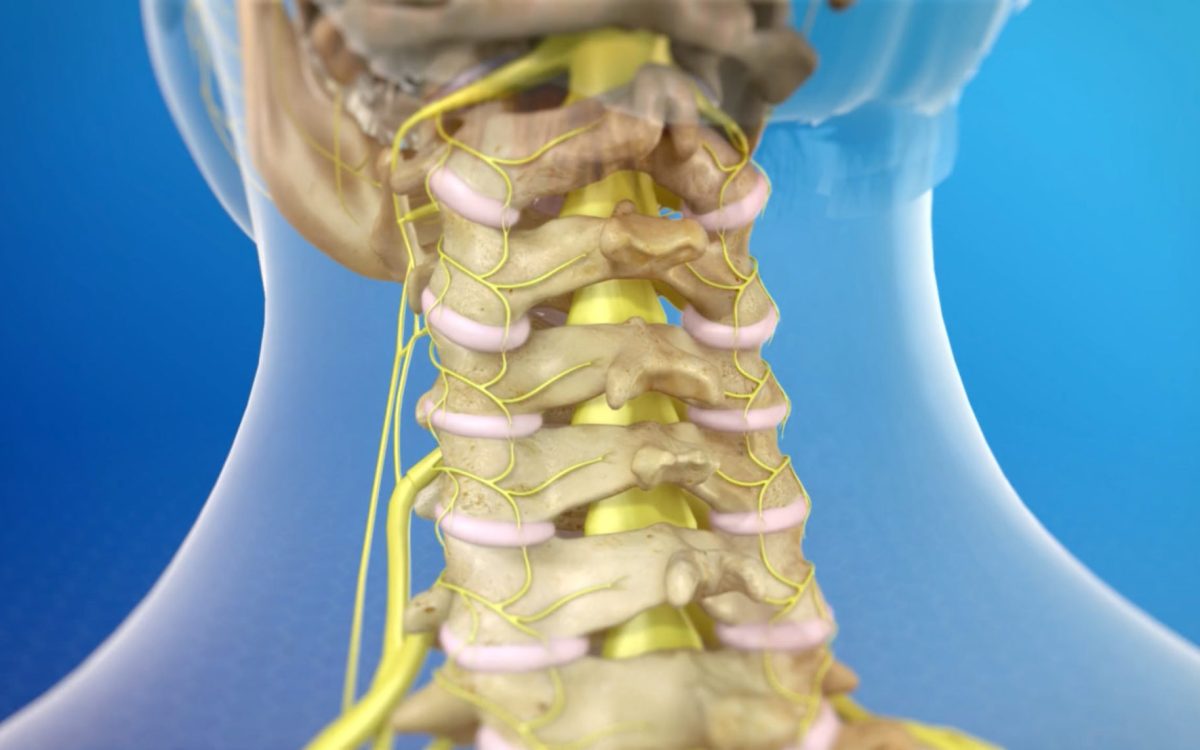
A neck ablation, also known as a cervical facet radiofrequency neurotomy, is a minimally invasive procedure used to relieve chronic neck pain caused by arthritis or injury. During the procedure, a needle is guided to the affected nerves in the neck and a radiofrequency current is used to damage the nerves, thus interrupting the pain signals being sent to the brain.
The level of pain experienced during a neck ablation can vary from person to person. Some patients may feel only mild discomfort, while others may experience moderate to severe pain during and after the procedure. The pain is generally well-tolerated with the help of local anesthesia and sedation used during the procedure.
After the neck ablation, patients may experience some soreness or discomfort at the site of the injection, as well as some numbness or tingling in the neck and shoulders. These side effects are usually temporary and can be managed with over-the-counter pain medications.
Overall, while a neck ablation may cause some discomfort and soreness, the pain relief benefits it offers can outweigh the temporary discomfort experienced during the procedure. It is important for patients to discuss any concerns or questions they have about the procedure with their healthcare provider before undergoing a neck ablation.
How long does nerve ablation procedure take?
The procedure usually takes an hour or less.
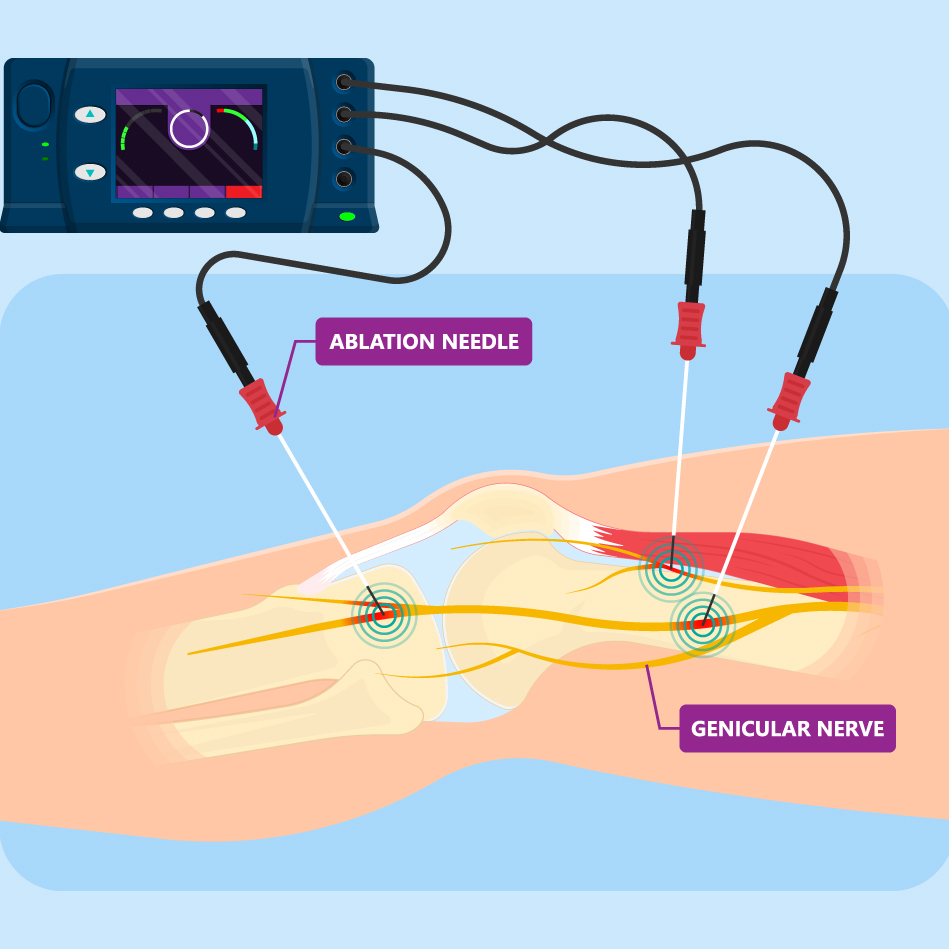
Does neck ablation hurt?
Overall, you may feel some mild discomfort or pressure during the procedure, but it should not be painful. You may have some discomfort during the testing and stimulation part of the procedure.
Are you sedated during a nerve ablation?
The patient remains awake and aware during the procedure to provide feedback to the physician. A low dose sedative, such as Valium or Versed, is usually the only medication given for this procedure.
Can you walk after nerve ablation?
Most patients can walk around immediately after the procedure. After being monitored for a short time, you can usually leave the office or suite. Someone must drive you home.
How to treat patellar tendon lateral femoral condyle impingement?
Non-surgical treatment consists of rest, ice, compression, and elevation (RICE protocol); all assist in controlling pain and swelling. Non-steroidal anti-inflammatory medications may be prescribed to reduce pain.
Is it OK to walk with patella subluxation?
When you have a patella subluxation, the kneecap still tracks in the groove and you can still walk, but it may feel uncomfortable or unsteady, and you may hear a popping noise as it moves. A patellar subluxation can result from injury or from general looseness in the joint (patellar instability).Aug 3, 2021
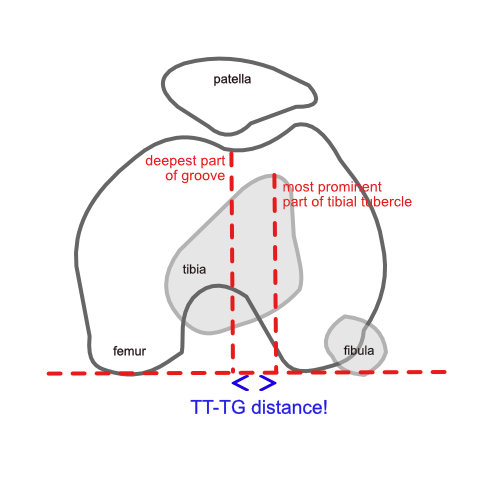
What is the TTG measurement of the knee?
Tibial tuberosityTibial tuberosityThe tuberosity of the tibia, tibial tuberosity or tibial tubercle is an elevation on the proximal, anterior aspect of the tibia, just below where the anterior surfaces of the lateral and medial tibial condyles end. Tuberosity of the tibia. Lateral aspect of right leg. (Tuberosity of tibia labeled at center right.)https://en.wikipedia.org › wiki › Tuberosity_of_the_tibiaTuberosity of the tibia – Wikipedia-trochlear groove (TT-TG) distance is a measure of lateralization of the tibial tuberosity in relation to femoral trochlea.
How do you treat Wiberg type 2 patella?
Conclusion: Recurrent dislocation of patella-Wiberg Type II, can be controlled by physiotherapy which includes a course of faradic stimulation to quadriceps and regular strengthening exercises of the knee extensors.
What is the TT to TG distance?
The TT-TG distance represents the radiographic measurement of the quadriceps vector, which represents a lateral force displacement on the patella during knee motion. It is > 20 mm in patients with recurrent patellar dislocations, as compared with 13 mm in control subjects.