Knowing the difference between a herniated disc and a pinched nerve can help in understanding the underlying cause of certain symptoms. Both conditions can result in similar symptoms, such as pain, numbness, and weakness. However, a herniated disc and a pinched nerve are two distinct conditions with different origins.
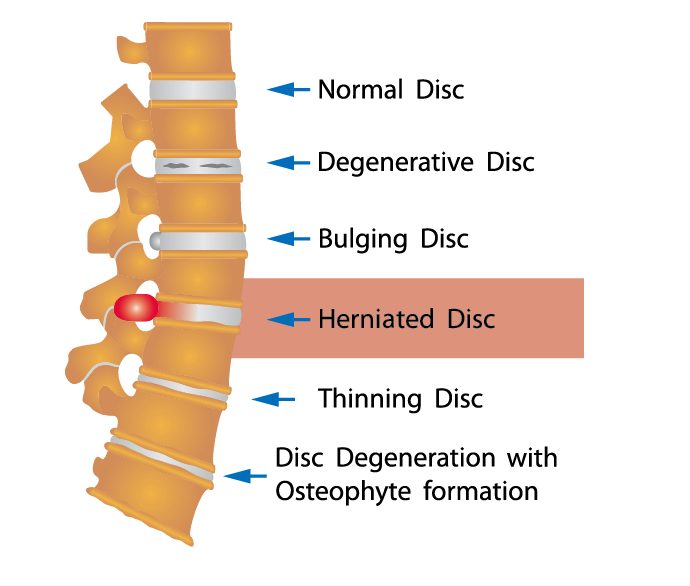
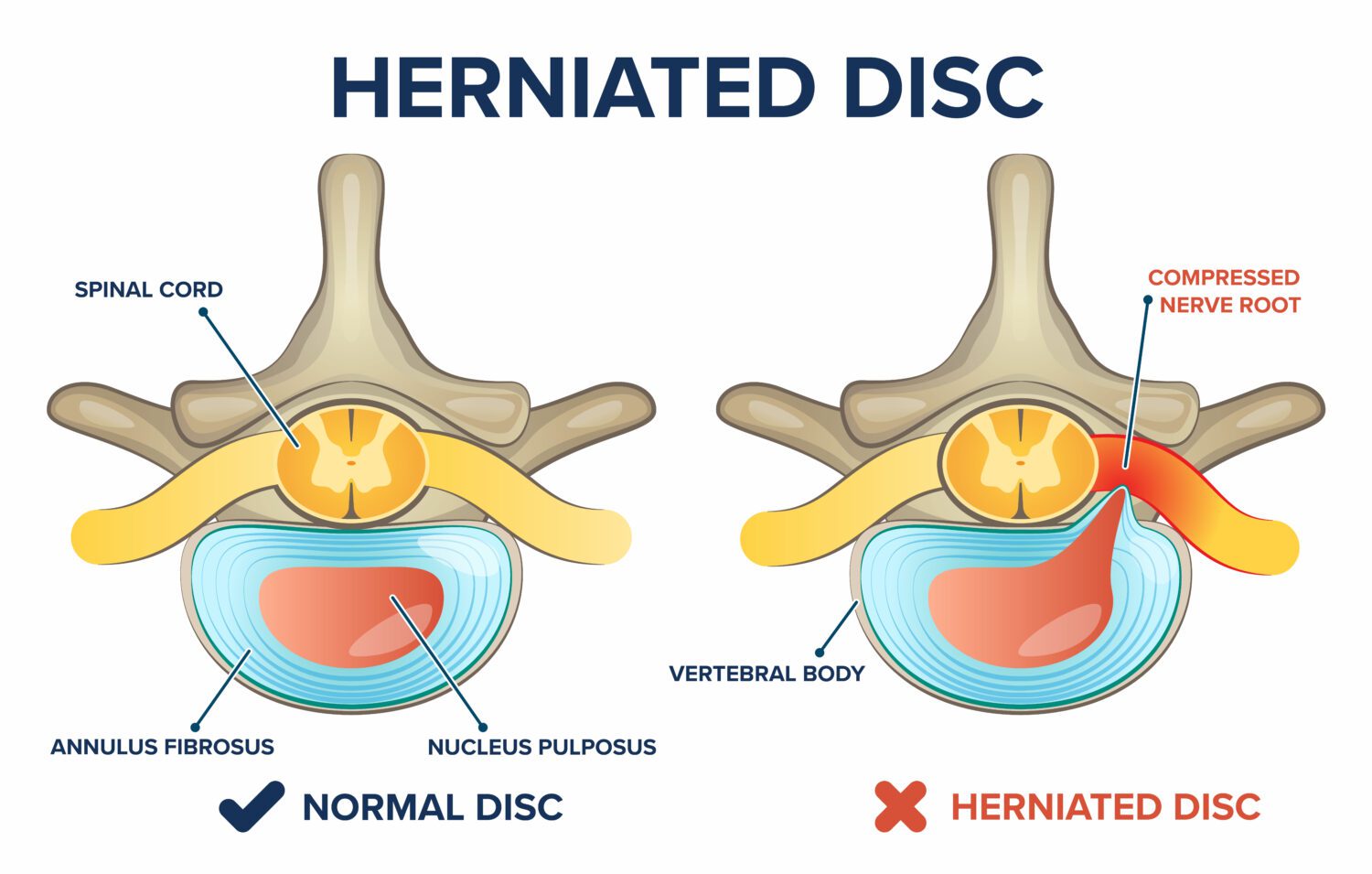
A herniated disc occurs when the soft inner material of a disc, located between the bones of the spine, pushes through the tough outer layer. This can cause compression or irritation of nearby nerves, leading to symptoms. The common causes of herniated discs include age-related degeneration, traumatic injury, and repetitive strain.
On the other hand, a pinched nerve, also known as nerve compression or nerve impingement, occurs when excessive pressure is exerted on a nerve by surrounding tissues, such as bones, muscles, tendons, or ligaments. This compression can disrupt the normal functioning of the affected nerve, resulting in symptoms like pain, tingling, and muscle weakness.
To determine whether one has a herniated disc or a pinched nerve, a medical evaluation is necessary. A healthcare professional will perform a thorough physical examination, review medical history, and request diagnostic tests like X-rays, MRIs, or CT scans.
Common symptoms of a herniated disc might include radiating pain, numbness, or weakness in the area of the body connected to the affected disc. Additional symptoms may include localized pain in the back or neck, muscle spasms, and difficulty with specific movements or positions.
In contrast, symptoms of a pinched nerve often involve pain, tingling, or numbness that radiates along the path of the affected nerve. This can lead to weakness in specific muscles supplied by the compressed nerve, decreased reflexes, and reduced sensation in the innervated area.
In conclusion, a medical evaluation and diagnostic tests are essential to differentiate between a herniated disc and a pinched nerve. By understanding the underlying cause of the symptoms, appropriate treatment can be administered to alleviate pain, improve function, and prevent further complications.
Can you physically feel a herniated disc?
If you have a bulging spinal disc, you may be wondering if you can physically feel it. You are not likely to be able to feel the disc itself, since it is located between the bones of your spine. However, you may be able to determine the affected area by touching various points along your back that you can reach.Dec 9, 2022
Can a herniated disk feel like a pulled muscle?
Slipped discs are a lot more focused than a strained muscle. The pain will likely be sharp and radiating, as opposed to a localized, aching pain of muscle. Because the disc puts pressure on the spinal cord, there will also be a neurological symptom, such as tingling or numbness.Jan 7, 2024
How do you tell if back pain is muscle or disc or nerve?
The Difference Between Muscle and Disc Pain Muscle pain will feel like post-workout soreness, while disc pain will feel debilitating and tingly. It is helpful to know the difference before you see your doctor so you can accurately describe the pain to them.
How do I know if I herniated my disc?
Some common symptoms of a herniated or slipped disc include: Pain that occurs on one side of the body. Sharp pain in one part of the leg, hip, or buttocks and numbness in other parts. You may also feel pain or numbness on the back of the calf or sole of the foot.
How long does it take to recover from a percutaneous discectomy?
While everyone’s recovery times differ, most patients can return to their regular jobs and pastime activities in about a week. Another advantage of percutaneous discectomy would be that it’s a minimally invasive alternative to surgery for treating spinal pain brought on by disc herniation.
Is lumbar discectomy major surgery?
Yes, a diskectomy can be a major surgery. But there are a few minimally invasive surgical approaches that are less major than an open diskectomy in terms of the days you spend in a hospital recovering.
What are the disadvantages of percutaneous discectomy?
– Reaction to anesthesia.
– Spinal cord compression.
– Excessive bleeding.
– Infection.
– Failure to remove all targeted disc tissue.
How soon can you walk after discectomy?
Three days after surgery Several short walks should be taken each day, and care should be taken to avoid prolonged, slouched sitting and heavy or repetitive lifting. You may experience slight pain around your surgical incision as it is healing; this is normal.
Is a percutaneous discectomy considered surgery?
A percutaneous discectomy is normally a safe, minimally-invasive, and effective surgical procedure.