Title: ICD-9 Codes for Low Back Pain: An Overview
Introduction:
Low back pain (LBP) is a prevalent musculoskeletal condition that affects millions of individuals worldwide. Accurate coding of LBP plays a crucial role in ensuring proper diagnosis, treatment, and reimbursement for healthcare services. In this article, we provide an overview of the International Classification of Diseases, 9th Revision (ICD-9) codes associated with low back pain.
Body:
The ICD-9 codes associated with low back pain depend on the underlying cause or specific symptoms. However, the most commonly used codes are as follows:
1. 722.10 – Displacement of Lumbar Intervertebral Disc without Myelopathy:
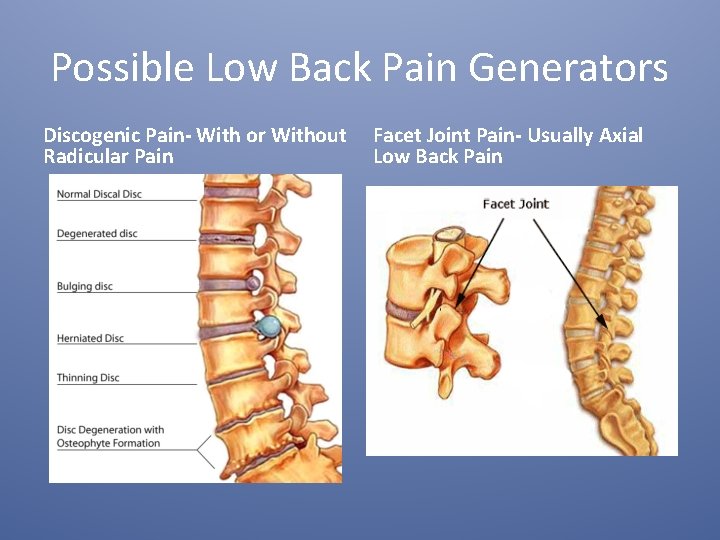
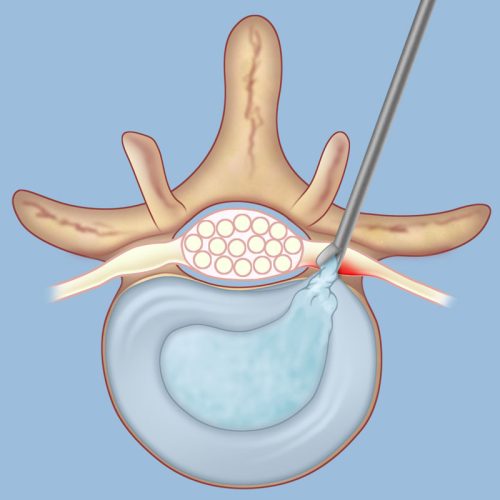
This code is used when a lumbar intervertebral disc is displaced, causing low back pain, without any associated myelopathy (spinal cord dysfunction). It is often a result of degenerative changes in the spine or disc herniation.
2. 724.2 – Lumbago:
Lumbago refers to non-specific low back pain that does not have a clear underlying cause. It is characterized by pain in the lower back region without radiation to the legs. This code is often used when the cause of pain is unknown or when there is no evidence of disc displacement or other specific conditions.
3. 721.3 – Lumbosacral Spondylosis without Myelopathy:
Spondylosis refers to degenerative changes in the spine, particularly in the lumbar and sacral regions. This code is used when these changes cause low back pain without associated myelopathy.
4. 846.0 – Sprains and Strains of Sacroiliac Region:
Sacroliliac (SI) joint sprains or strains can cause low back pain, commonly felt on one side of the low back. This code is used when the primary cause of pain is related to SI joint dysfunction.
Conclusion:
Accurate coding of low back pain using the appropriate ICD-9 codes is crucial for healthcare providers to effectively diagnose, treat, and manage this prevalent condition. Understanding the various codes associated with specific underlying causes or symptoms enables proper categorization and documentation of patient records, ensuring optimal care and appropriate reimbursement. However, it is important to note that the ICD-9 system has been replaced by the ICD-10 system for coding purposes, and healthcare professionals should now utilize the ICD-10 codes when documenting and coding low back pain cases.
What is diagnosis code M54 50?
M54. 50, Low back pain, unspecified.Sep 7, 2021
What is the ICD-10 code for pain over lower back?
2024 ICD-10-CM Diagnosis Code M54. 5: Low back pain.
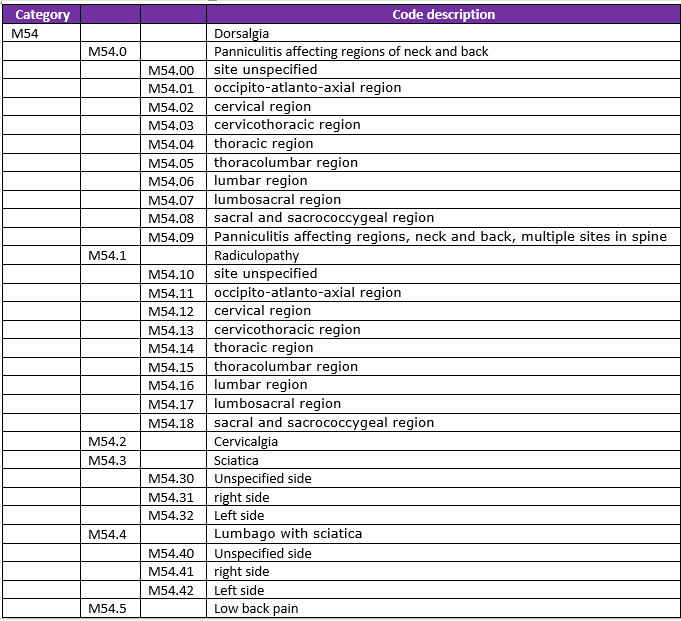
What is the new ICD-10 code for low back pain?
2024 ICD-10-CM Diagnosis Code M54. 5: Low back pain.
What causes lower back pain on left side?
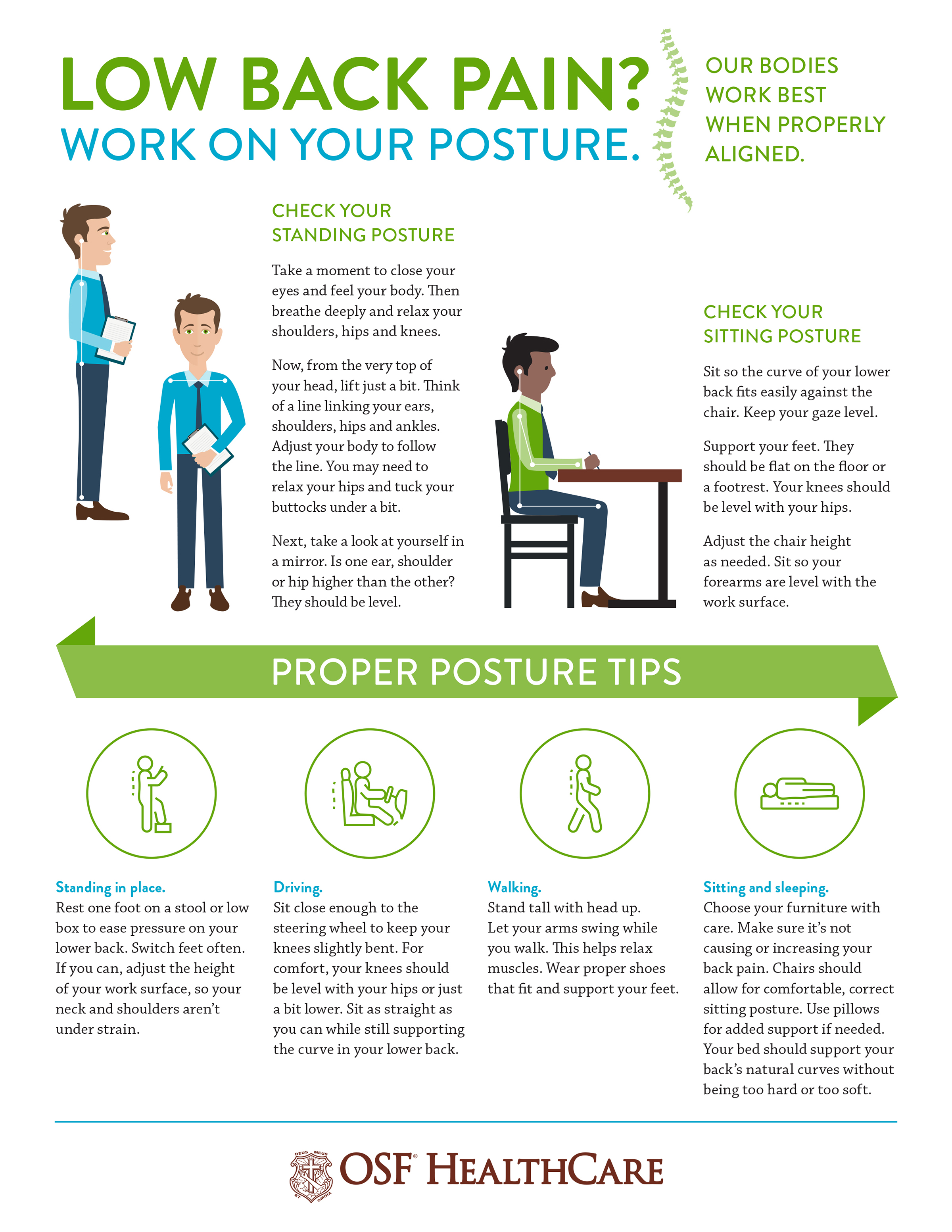
Pain in the lower left back could indicate a problem with the muscles, joints, mid-back, or organs in the pelvic area. Common sources of pain include muscle injuries, kidney problems, and arthritis. Back pain is a common occurrence and can have many possible causes.

When should I be worried about lower back pain?
If the pain lasts four weeks or longer. If the pain keeps getting worse as time goes by. If you are experiencing other symptoms, such as fever, major weight loss or weight gain, loss of function or weakness in extremities, bladder problems, etc.
How can you tell if back pain is muscular or something else?
Dull, achy low back pain Strained muscles usually feel sore, tight, or achy. Pain that feels hot, tingling, or electric is more likely caused by an irritated nerve root, not a pulled muscle.
How can I tell what kind of back pain I have?
Acute back pain happens suddenly and usually lasts a few days to a few weeks. Subacute back pain can come on suddenly or over time and lasts 4 to 12 weeks. Chronic back pain may come on quickly or slowly and lasts longer than 12 weeks and occurs daily.